Borderline Personality Disorder: not what social media claims it is
Like any other mental health disorder, Borderline Personality Disorder (BPD) is misunderstood and, at times, demonized. The only difference between this disorder and other disorders such as Major Depressive Disorder (MDD) or Generalized Anxiety Disorder (GAD) is that BPD falls under the mental health category of Personality Disorders.
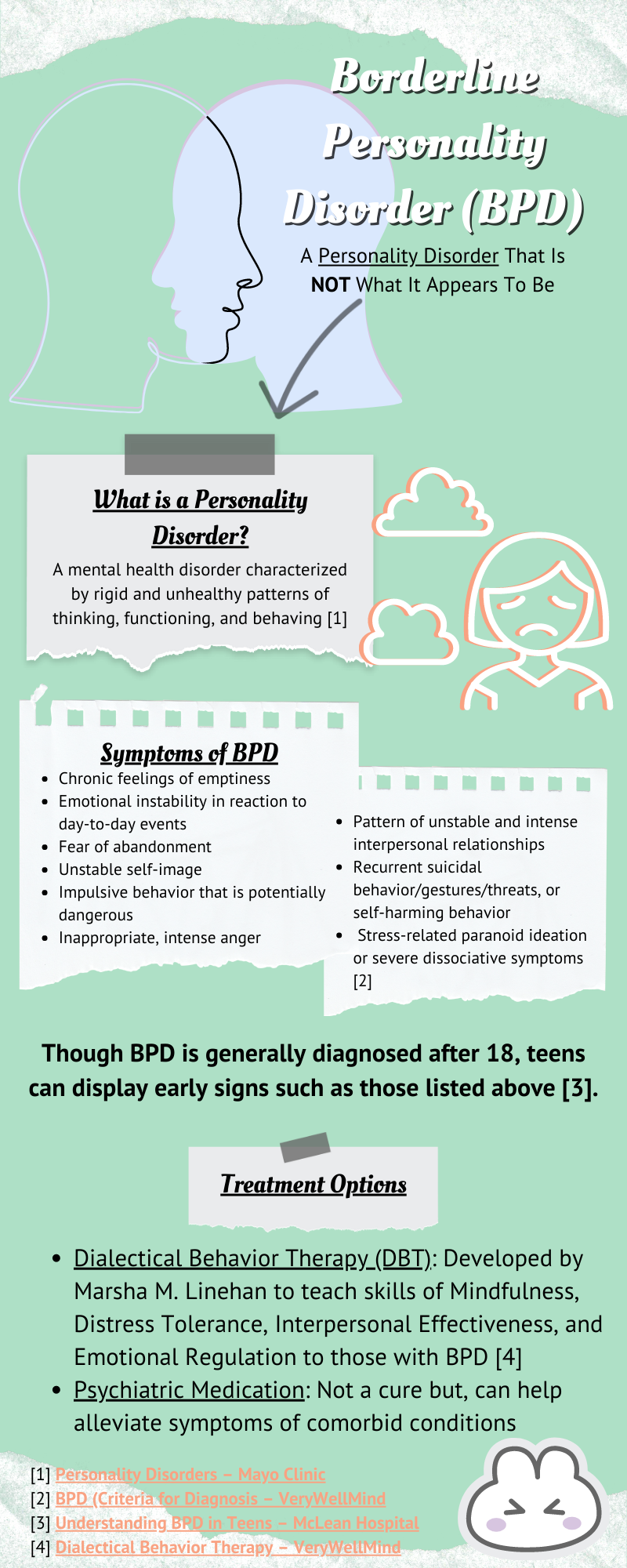
Now, what are Personality Disorders?
Personality Disorders are mental health disorders characterized by rigid and unhealthy patterns of thinking, functioning, and behaving. They are grouped into 3 categories: cluster A, cluster B, and cluster C personality disorders.
Cluster A disorders center around odd, eccentric thinking or behavior. This category consists of Paranoid Personality Disorder, Schizoid Personality Disorder, and Schizotypal Personality Disorder.
Cluster C disorders focus on symptoms of anxiety and fearful thinking or behavior. They include Avoidant Personality Disorder, Dependent Personality Disorder, and Obsessive-Compulsive Personality Disorder (not to be confused with Obsessive-Compulsive Disorder).
Onto cluster B which includes BPD. Disorders in this cluster are defined by their dramatic, overly emotional or unpredictable thinking/behavior. Other disorders that fall under this category are Antisocial Personality Disorder, Histrionic Personality Disorder, Narcissistic Personality Disorder, and, of course, Borderline Personality Disorder.
Onto symptoms of BPD and screenings to help see if you display symptoms.
As previously mentioned, BPD is under the category of dramatic, overly emotional or unpredictable actions/thoughts. Symptoms of this disorder, as listed by the DSM-5, are as follows:
Chronic feelings of emptiness
Emotional instability in reaction to day-to-day events (e.g., intense episodic sadness, irritability, or anxiety usually lasting a few hours and only rarely more than a few days)
Frantic efforts to avoid real or imagined abandonment
Identity disturbance with markedly or persistently unstable self-image or sense of self
Impulsive behavior in at least two areas that are potentially self-damaging (e.g., spending, sex, substance abuse, reckless driving, binge-eating)
Inappropriate, intense anger or difficulty controlling anger (e.g., frequent displays of temper, constant anger, recurrent physical fights)
Pattern of unstable and intense interpersonal relationships characterized by extremes between idealization and devaluation (also known as “splitting”)
Recurrent suicidal behavior, gestures, or threats, or self-harming behavior
Transient, stress-related paranoid ideation or severe dissociative symptoms
Before taking these screenings, remember that this is NOT a diagnostic tool and that after taking these test, you should talk with your primary care physician about your concerns.
Borderline Personality Disorder (BPD) Test (TalkSpace)
3 Minute BPD Self-Assessment (Psycom.net)
Borderline Personality Test (Psych Central)
For a formal diagnosis of BPD, you first need to seek out the help of a mental health professional. After speaking to them about your concerns, they will conduct an extensive interview to determine if you may have BPD.
Being a teenager is full of ups and downs, but, when does it come to the point of showing early signs of BPD?
Similar to the symptoms of BPD, the youth display unpredictable, irrational patterns of thought or behavior that can be indicative of the condition. Teens can show difficulty sustaining friendships or romantic relationships. As they are teenagers, emotional outbursts are regarded as a symptom of their age. However, when it comes to the point where the teen has these outbursts of intense emotions and takes longer than their peers to get back to their personal emotional baseline, there is a concern that the teen may have BPD.
Acknowledging the symptoms is step 1, following this are different treatments that can alleviate the symptoms of BPD.
There is NOT a “cure” for Borderline Personality Disorder, however, there is the possibility of not qualifying for the disorder. This means that any symptoms felt are managed by therapy and/or medication. You can recover from a BPD diagnosis.
The first treatment for BPD is Dialectical Behavior Therapy (DBT), created by Marsha M. Linehan. Linehan developed this therapy as a result of the treatment that was previously put in place to treat BPD (which she also was diagnosed with). DBT is centered around 4 topics/skills.
Mindfulness – This deals with focusing on the moment, “living” in it. It allows for your focus to shift to healthy coping, rather than catastrophizing about the future or ruminating on negative thoughts.
Distress Tolerance – As the name indicates, it deals with tolerance. This tolerance is usually for an emotional crisis. Techniques commonly taught to help during a crisis are using distractions and practicing self-soothing.
Interpersonal Effectiveness – This teaches you how to be assertive in your relationships while also keeping the relationship healthy and positive.
Emotional Regulation – This deals with effectively navigating the intense mood swings by teaching you healthy management skills.
Alongside this, psychiatric medication management is used. These medications are not cures for BPD, rather they are used to alleviate any symptoms from comorbid disorders. Some comorbid disorders are listed below.
Major Depressive Disorder (MDD)
Bipolar I or Bipolar II Disorder
Anxiety Disorders
Post-Traumatic Stress Disorder (PTSD)
Substance Use Disorders
Eating Disorders
Other Personality Disorders
Other resources that can help with your mental health journey.
Borderline Personality Disorder (NAMI: National Alliance on Mental Illness)
BPD Overview (National Education Alliance for Borderline Personality Disorder)
Borderline Personality Disorder (Mental Health America)