The Stress-Vulnerability Model and Why I Should Care
Learn about the relationship between our biology and stress, and how you can use it to your benefit
For so many teens and young individuals living with mental health challenges, I have seen it in their eyes. The look of despair. Feelings of hopelessness. The heartbreaking idea that perhaps, they are “broken” by their mental illness. That this is just how it is going to be for their whole life, and suffering from their symptoms is inevitable and uncontrollable. There is nothing they can do.
I do the work that I do because I want to be able to challenge that notion. To change that self-defeating thought that we are “stuck” on a path that we cannot control. Sure, life happens. Mental health challenges happen, and they occur often to individuals from all walks of life. The difficulty in part lies in the reality that we still struggle to talk openly about emotional health openly. It often seems that we are alone in our feelings, thoughts, and experiences. As a result, clinical disorders such as depression, anxiety, trauma, and serious mental illness are misunderstood and creates a fear of the unknown.
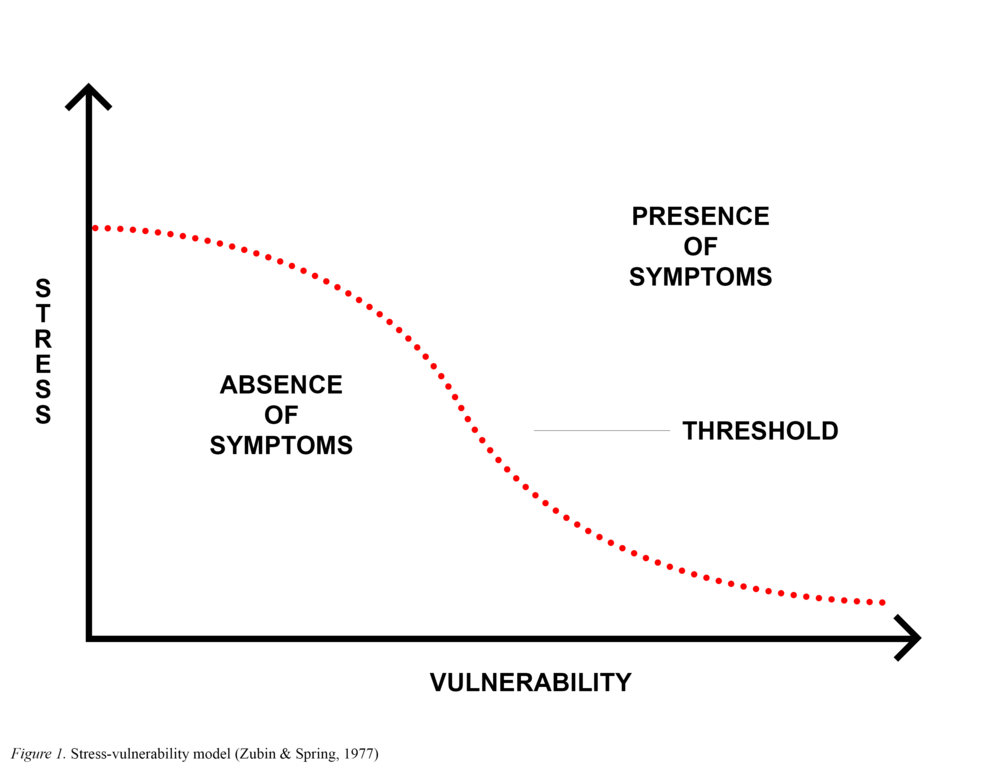
This is where knowledge and psychoeducation about what the research says on the topic of mental health conditions and symptoms are key. When thinking about clinical symptoms such as early psychosis, one of the well-known theoretical models to help us understand how and why symptoms of psychosis occurs is the stress-vulnerability model by Zubin & Spring (1977).
According to the stress-vulnerability model, all individuals exist on a spectrum of having different levels of biological vulnerability (from low to high). Environmental stress is measured on the other part of the axis, and also ranges from low to high levels of stress. In this model, a curved threshold exists, delineating the presence versus absence of clinical symptoms.
Here’s how the model works: For instance, a person is considered to have lower biological vulnerabilities when they have no personal or family current/history mental health disorders, trauma or adverse childhood experiences, genetic risks and/or medical/developmental issues. Hence, they would be found in the lower end of the spectrum. For such an individual to begin having symptoms of psychosis, they would likely have to experience a significant amount of stressors (i.e., work/school, social relationships, etc.) over time or in their daily life.
In comparison, for a person who has multiple instances of biological and genetic load (e.g., prenatal complications, history of neglect, mood disorders, family trauma), the likelihood or risk of experiencing the presence of psychosis symptoms when they are faced with elevated stress is much higher, due to the lower stress threshold they are needing to meet. So it is easier for individuals who have a higher biological vulnerability to become easily affected by their environmental stress and result in symptoms. To learn more about the research on the relationship between trauma and psychosis, read my article here.
So what do I do with this information? How does this help me?
The purpose of this entry is to offer hope. If you or someone you know or love is experiencing mental health challenges such as psychosis, know that there is something that can be done. It is not all biologically predetermined that individuals with mental health disorders or clinical symptoms are “stuck.” Biology certainly accounts for part of the equation, but not all of it. Instead, I want to highlight the importance of understanding the other part of the theoretical model, that is, stress.
Because here, there is definitely something that we can do. Through better self-care routines, improved stress management, and learning more effective coping skills, we can wield some control over our lives and health status. We can make more adaptive choices in our daily lifestyle patterns, and through help-seeking (such as individual therapy and/or medication management), we can begin to shift our focus away from the risk factors of illness to putting more of our efforts into boosting our protective factors (such as increased social support, role functioning in the community, physical health and wellness). We can begin to help ourselves.